Case control study: incidence and risk factors of postpartum haemorrhage in primigravida.
Yusof J1*, Mohammed M2, Fuad NA3
1. Masters of Obstetrics & Gynecology, Faculty of Medicine, University Technology of MARA, Sungai Buloh, Malaysia
2. Masters of Public Health, Faculty of Medicine, University Technology of MARA, Sg Buloh, Malaysia
3. Masters of Obstetrics & Gynecology, Sungai Buloh Hospital, Malaysia
Corresponding author:
Juliana Yusof, Masters of Obstetrics & Gynecology, Faculty of Medicine, University Technology of MARA, Sungai Buloh, Malaysia
Received: September 29, 2021
Accepted: October 11, 2021
Published: October 11, 2021
1. Abstract
1.1.Introduction: According to WHO, postpartum haemorrhage is defined as blood loss of more than 500mL following vaginal delivery. Postpartum haemorrhage is still one of the leading causes of maternal deaths in Malaysia. The risk factors of postpartum hemorrhage in this study was divided into three which were pre-pregnancy, antenatal and intrapartum. Methods: We performed a case control study to identify the risk factors for post-partum hemorrhage among primigravida in Sungai Buloh Hospital from 2016 to 2018. From the calculation that we have done by using simple random sampling method, the required respondents were 150 for both case and control. The data collection method was in an audit form. The data that we have obtained was entered using SPSS 21 (a statistical software). Results: From 2016 to 2018, we had identified 75 cases and 75 random controls of postpartum hemorrhage among primigravida. The risk factors associated with post- partum hemorrhage in primigravida that is significant with p value less than 0.05 were age (p=0.001), occupation mainly self-employed (p=0.000), anemia during antenatal (p=0.000), uterine fibroid (p=0.007), prolonged labour more than 8 hours (p=0.005), instrumental delivery (p=0.001), extensive vaginal wall tear (p=0.009), cervical tear (p=0.013), 3rd and 4th degree tear (p=0.006), uterine atony (p=0.000) and vascular lower segment during caesarean section (p=0.029).
1.2.Conclusion: The results showed that the risk factors for post-partum hemorrhage in primigravida were age, occupation (self-employed), antenatal anemia, uterine fibroid, prolonged labour more than 8 hours, instrumental delivery, extensive vaginal wall tear, cervical tear, 3rd and 4th degree tear, uterine atony and vascular lower segment during caesarean section.
Introduction
For centuries, the biggest concerns in pregnancy would be the mother and the baby, where it will be either one to survive the whole pregnancy or both of them. In United Kingdom, the most recent Confidential Enquiry into Maternal Deaths (CEMD) reports indicates that from 2009 till 2012, 357 women died during or within 6 weeks of the end of their pregnancy. This represents a decrease in the maternal mortality ratio (MMR) where in 2006 to 2008 it was 11, while in 2009 to 2012 it was 10.12 per 100,000 live births, mainly due to direct obstetric causes [3]. In Malaysia however since embarking on CEMD in 1991, the maternal mortality ratio has declined from 44 in 1991 to 27 per 100,000 live births in 2011 [4].
The causes of maternal deaths can be divided into direct causes or indirect causes. Direct causes from complications during pregnancy are the prime suspects for maternal deaths which includes obstetric embolism, postpartum haemorrhage and hypertensive disorders in pregnancy. Indirect causes resulted in about 17% of death whereby heart diseases is the most common cause. Out of all these causes, postpartum haemorrhage is still one of the leading causes of maternal deaths in Malaysia. There were 27 deaths in 2001, 16 deaths in 2003, 17 deaths in 2005, 24 deaths in 2006, 23 deaths in 2007 and 26 deaths in 2008 [2].
According to WHO, postpartum haemorrhage (PPH) is defined as blood loss of more than 500mL . A loss of these amounts within 24 hours of delivery is termed early or primary PPH, whereas such losses are termed late or secondary PPH if they occur 24 hours after delivery until 12 weeks postpartum. The amount of blood loss required to cause hemodynamic compromise will depend on the pre-existing condition of the woman. Hemodynamic compromise is more likely to occur in conditions such as anemia or volume contracted states. All women who carry a pregnancy beyond 20 weeks’ gestation are at risk for PPH and its sequelae [1].
Risk factors of postpartum hemorrhage can be divided into three which are pre- pregnancy, antenatal and intrapartum. There are quite a lot of risk factors for development of postpartum hemorrhage that need to be elicited from history taking. Example are anemia, hemophilia A, hemophilia B and Von Willebrands disease. During antenatal, the example of risks that were identified were severe preeclampsia with thrombocytopenia, maternal obesity and thromboprophylaxis drugs. The risk factors that were studied intrapartum were delivery by ceasarean section, retained placenta, genital tract trauma, prolonged labor for more than 8 hours, delivery of a macrosomic baby of more than 4kg, operative vaginal delivery and pyrexia in the intrapartum period [1].
Objective
• To determine the risk factors for postpartum haemorrhage in primigravida at Sungai Buloh Hospital (HSgB) from 2016-2018 during antenatal and intrapartum period.
Methodology
This was a retrospective case control study conducted at Hospital Sungai Buloh (HSgB), Sungai Buloh, Selangor conducted from 1st January 2016 to 15th July 2018. We identified 150 patients for cases and controls. The definition of cases is primigravida deliver at HSgB from 1st January 2016 to 15th July 2018 with PPH. PPH is defined as more than 500ml blood loss during delivery in normal delivery and more than 1000ml in caesarean section. Meanwhile, the definition of control is primigravida that delivered at HSgB from 1st January 2016 to 15th July 2018 without PPH.
We calculate our sample size by using formula! “($%!”) ( !) ($%!)) 𝑋 (𝑋 + 𝑋 ) (!”%!)))
By taking α = 0.05, 80% power of study and proportion of group 1 was 41.7% from study by Chandrika et al., (2014) and the proportion of group 2 was 19.3% from study by Tan et al., (2013), the sample size needed will be 62 in each group. After adjusting 20% attrition rate, the minimum sample required in this study will be 75 in each group.
We selected cases and control from delivery book of HSgB. The first 75 patient that had been chosen in the delivery book will be taken in this study for both cases and controls. The patient’s demographic, antenatal and intrapartum data were retrieved from hospital computer system based on their registration number. In our audit form, the antenatal risk factors were anemia, placenta previa, polyhydramnios, multiple pregnancy, booking body mass index (BMI)>30kg/m2, excessive weight gain, uterine fibroid, magnesium sulphate MgSO4 infusion, thrombocytopenia/bleeding disorder, Induction of Labour (IOL) with prostin, prophylaxis clexane and aspirin. Risk factors for intrapartum identified were method of delivery, abruptio placenta, precipitated labour less than 3 hours, poor progress of labour more than 8 hours , prolonged second stage more than 1 hour, instrumental delivery, extensive vaginal wall tear, cervical tear, 3rd and 4th degree tear, retained placenta, macrosomic baby >4kg and uterine atony. For intraoperative, the risk factors identified were Disseminated Intravascular Coagulopathy ( DIVC), vascular lower segment during caesarean section, classical caesarean section and extended tear of incision during caesarean section.
The data was then entered into SPSS version 21 for analysis. In describing the socio-demographic and first pregnancy details, measure central tendencies (means) were used. For categorical data, frequencies were computed. Chi square or Fisher’s test was used to compare proportions to determine strength of association between PPH and its risk factors during antenatal, intrapartum and intraoperative. A p -value less than 0.05 used to determine association between variables was considered statically significant.
Results
Total number of patients in this study were 150 of which 75 of them were cases and another 75 patients were control. The patient’s data who delivered at Sungai Buloh Hospital from 1st January 2016 till 15th July 2018 were retrieved. Cases and control were selected by using simple random sampling using random number computer generated.
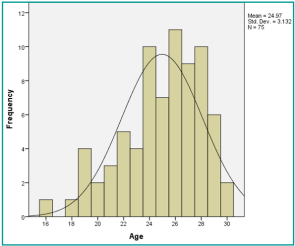
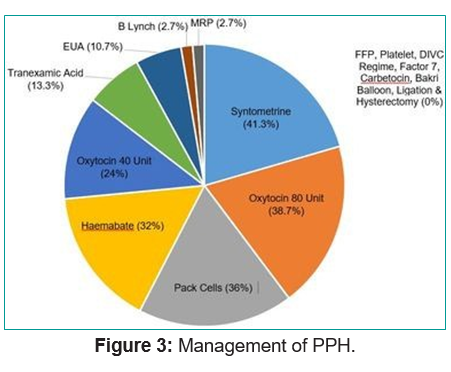
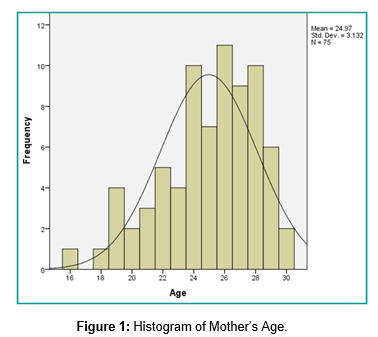
Table 1 shows the socio-demographic details of both cases and controls, where we focused on age groups from 17 to 35 years old. The mean age for cases and controls was 26.57 years (SD 4.03) and 24.49 (SD 3.54) years old respectively as shown in (Figure 1). Most of the patients were Malays which comprises of 80%, 9.3% were Chinese and 3.3% were Indians. In terms of occupations, 48% of cases were self- employed of which it was significantly associated with post-partum haemorrhage (p<0.05). Other socio-demographic characteristics are shown as below.
Table 2 represents blood group and gestational age of delivery details of both cases and control subjects. This study showed that 73.3% of cases had done their booking compared to 49.3% of control. Other than that, majority of cases blood group was type O (45.3%) followed by B (28%), A (21.4%) and AB (4%) while for control, majority of them had type A (34.7%) followed by O (33.3%), B (20%) and AB (5.3%). However, there was no significant association of blood group and PPH.
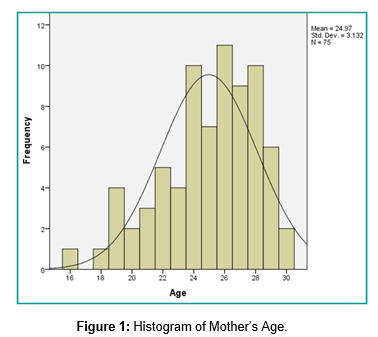
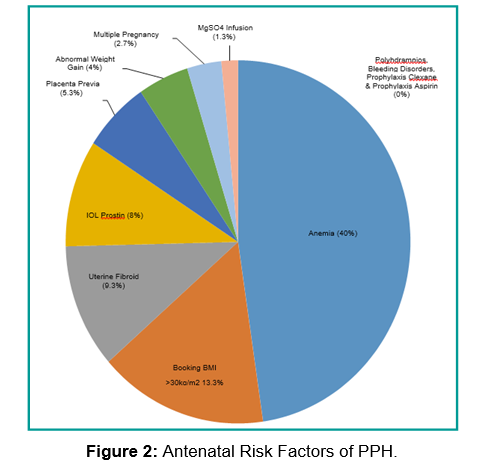
Our study revealed that anemia is the most common factor that lead to postpartum hemorrhage (40%) as shown in Figure 2 with p value of <0.05 as shown in Table 3. The second commonest cause was uterine fibroid (9.3%) followed by placenta praevia. However placenta praevia was not statistically significant.
From Table 4, PPH incidence was significantly higher in instrumental delivery (18.7%) compared to control (6.7%). Other than that, 3rd and 4th degree tear, prolonged labour more than 8 hours, extensive vaginal wall tear, cervical tear and uterine atony were significantly associated with post-partum haemorrhage as all of the p- value were <0.05.
Table 4a revealed that anemia was profound most in uterine ny, and if compared with control, anemia is statistically significant to cause uterine atony in primigravida. In Table 4a (i), uterine atony most commonly occurred in patient delivered by Caesarean section.
Table 4b revealed that other possible risk factors leading to uterine atony as above in primigravida were not statistically significant.
Table 4c revealed that genital tract trauma such as vagina wall tear, cervical tear and 3rd or 4th degree tear occurred more commonly in patient who delivered via spontaneous vagina delivery (SVD) compared from instrumental delivery.
Table 4d revealed that instrumental delivery especially metal cup vacuum and forceps significantly causes PPH due to prolonged second stage as risk factor and not genital tract trauma eventhough prolonged second stage (in comparison with control) was not statistically significant to cause PPH in primid.
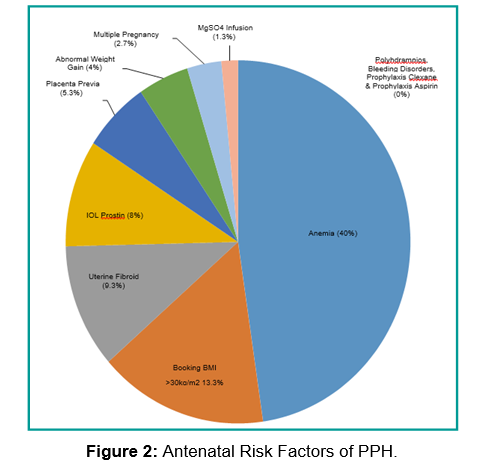
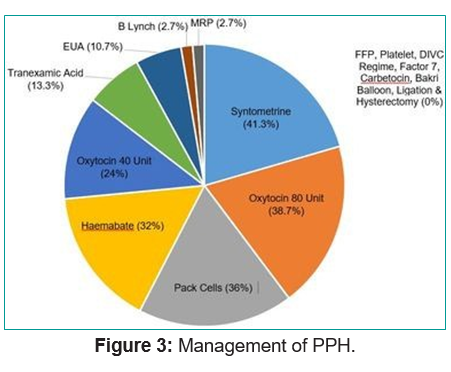
From Table 5, the most important intraoperative factor for PPH was vascular lower segment during caesarean section which was 6.7% which was significantly associated with post-partum haemorrhage with p value of 0.029. For the management of postpartum hemorrhage in Sungai Buloh Hospital, PPH was mainly managed it with uterotonic agents . Table 6 and Figure 3 revealed that oxytoxin 80unit (38.7%) and syntometrine (41.3%) were mainly used. Surgical management was uncommon, of which Examination Under Anaesthesia (EUA) prevalence was 10.7%, manual removal of placenta (MRP) was 2.7% and fortunately no hysterectomy was needed.
Discussion
In this case-control study, we evaluated risk factors for PPH in a primigravida. Assessing risk factors in retrospective manner is a limitation in this study. In order to minimize selection bias, we selected a number of cases of PPH according to our sample size and a random sample of controls from the same source population. There is a possibility that some cases were misclassified. Secondly, our sample size may not be sufficient to evaluate potential risk factors that are less frequent. Another limitation was limited by the missing data. Measures should be taken to ensure data entry is complete for a comprehensive analysis.
In this study, we limited the age group from 17-35 years old which differs to other study as we are focusing on primigravida who are mostly young. From our analysis, the commonest age group for PPH with primigravida were from age group of 26-30 years (41.3%) followed by age group of 21- 25 years old. From the socio- demographic details, patient’s occupation contributed to risk factors for PPH. A definition of woman’s health as defined by Koblinsky et al [10] stated “A woman’s health is her total wellbeing, not determined solely by biological factors and reproduction, but also the effects of work load, nutrition, stress, war and migration, among others” [11]. Therefore, from the results, self-employed was the highest factor to contribute to PPH which was similar to study done by Gregory Hella Ekane et al [12] followed by occupation in government sector, private and least housewife. This might be due to financial instability among self employed primigravida which could lead to stress.
The strongest risk factor during antenatal in our study was anemia during pregnancy which is same as the finding in Chandrika et al and Tan et al [6,7]. An explanation for the association between anemia and post-partum hemorrhage is uterine muscle hypoxia. Hemoglobin is the oxygen- carrying protein in blood. Anemia is the state of a reduction in hemoglobin levels, and therefore, in the blood’s oxygen- carrying capacity. After hours of maximal exertion, due to insufficient oxygen, the uterus will have inefficient uterine contractility hence leading to haemorrhage. Early detection of anaemia and timely correction is important to reduce morbidity associated with PPH. As shown in Table 4a, anemia was significantly associated with uterine atony.
Another risk factor that was significantly related to PPH in primigravida was presence of uterine fibroid. Based on study by Hee Joong Lee [17], the association between fibroid and postpartum hemorrhage was due to the fibroid will distort the uterine cavity and interfere with myometrial contractions leading to uterine atony and postpartum hemorrhage. Uterine dysfunction before the onset of active labor, such as uterine fibroid, overdistended uterus, scarred uterus, and infection, may result in delay of all stages of labor and thereby cause PPH [17]. To prevent PPH in patient with uterine fibroid, myomectomy can be considered prior to pregnancy. Several studies have reported that antepartum myomectomy can be safely performed in the first and second trimester of pregnancy [18].
According to Chandrika et al [6] delivery by emergency caesarean section carries the highest risk for severe post- partum hemorrhage which is consistent with this study, of which 45 out of 75 or 60% primigravida who delivered by caesarean section had PPH. Uterine atony contributed to 60% of blood loss in patient who delivered by Caesarean section as shown in Table 4a. Another study done by Waheed et al [18] also highlighted that Caesarean section and instrumental deliveries are more likely to be complicated by PPH. In this study, instrumental delivery carried higher prevalence of PPH (p<0.05) especially metal cup and forceps in primigravida who had prolonged second stage as shown in Table 4d . Hashim N et al revealed that primigravida has higher risk of prolonged second stage [5].
In this study, we found that the duration of active labor of more than 8 hours was associated with an increased risk of PPH (p<0.05) Nyflot et. al [16] stated that long lasting labor, including a prolonged first stage, may increase the risk of PPH by causing uterine atony due to prolonged regular contractions over several hours of labor will exhaust the uterine muscles and thereby reduce their contractility over time, causing uterine dysfunction [17].
Genital tract trauma that occurred during childbirth could lead to postpartum hemorrhage and in this study, we had identified that extensive vaginal wall tear, cervical tea, 3rd as well as 4th degree tear (p=0.006) were the risk factors to postpartum hemorrhage in primigravida. A study from Smith et.al, showed that these tears were closely related to shoulder dystocia, episiotomy, prolonged second stage of labour, macrosomic baby and instrumental delivery [13]. In nulliparous women at term, external cervical so remains stationary during the cervical shortening, but it quickly evolves once the cervical effacement is completed [14].
The next risk factor of postpartum hemorrhage in primigravida that was identified in this study was 3rd and 4th degree tear. Third and 4th degree tear occurs in about 3 in 100 women having a vaginal birth. It is slightly more common with a first vaginal birth, occurring in 6 in 100 women, compared with 2 in 100 women who have had a vaginal birth previously [11]. This is because the age related changes in the connective tissue decrease the ability of cervical, vaginal and perineal muscles to stretch as needed during delivery resulting in greater trauma to tissues, prolonged labor and diminished uterine contractility after delivery [13].
However surprisingly in this study, genital tract trauma majority occurred in patient who delivered by spontaneous vaginal delivery, not instrumental delivery as shown in Table 4c.
During intrapartum, uterine atony (48%) was the commonest cause of post-partum hemorrhage, this is the same as the finding in previous studies done [8-10]. After the placenta is delivered, these contractions help compress the bleeding vessels in the area where the placenta was attached. If the uterus has inefficient uterine contraction, bleeding from blood vessels tends to occur that can lead to post-partum hemorrhage. Uterine atony is treated initially by uterine massage, followed by uterotonic agents such as oxyctocin, syntometrine or hemabate that promote uterine contraction. Hence continuous training should be provided to all doctors and nursing staff on how to managing uterine atony as the uterus can be salvage easily.
The last risk factors that we had identified which has p value of <0.05 was vascular lower segment during caesarean section; 5 cases (p=0.029). A thick lower segment is usually encountered in elective cesarean sections performed before the onset of labor. Proportionate to the thickness, the incision will have to be larger and hence blood loss will be greater. Trying to arrest bleeding at that point with cautery or ligation is not advisable. One has to proceed to deliver the fetus and then tackle the bleeding. A thick lower segment may demand use of forceps or ventouse to facilitate delivery of the fetus [15].
Syntometrine administration is most commonly used to manage post-partum hemorrhage in this study in which there were 31 cases with 41.3% followed by oxcytocin 80 unit with 29 cases (38.7%). There are significant variations in practice but systematic review of all the available uterotonics for prevention of PPH found oxytocin to be the first choice and a recent Cochrane review supported this recommendation [20]. Syntometrine which is combination of ergometrine and oxytocin is more effective than oxytocin alone in preventing blood loss, however their side effects are more common, with increased levels of hypertension, nausea, and vomiting [19]. According to WHO [4], the use of oxytocin for active management of the third stage of labour is strongly recommended, because it reduces post-partum hemorrhage by more than 60%.
In this study, there was no maternal death in primigravida with PPH as Sungai Buloh Hospital has well-trained personnel and good facilities of managing postpartum haemorrhage.
Conclusion
In this study, the significant risk factors for post-partum hemorrhage in primigravida were age, self-employed, uterine fibroid, prolonged labor for more than 8 hours, antenatal anemia, instrumental delivery with prolonged second stage, extensive vaginal wall tear, cervical tear, 3rd and 4th degree tear, uterine atony and vascular lower segment. Anemia significantly causes uterine atony and hence should be corrected antenatally. In terms of instrumental delivery, silicone vacuum less commonly associated with PPH as compared from forceps and metal cup vacuum.
Further studies are needed for explanation of higher incidence of genital tract trauma in spontaneous vaginal delivery compared to instrumental delivery. Risk factors identified in our study could be considered in future studies such as examining risk prediction models for post-partum hemorrhage.
References
1. Saxena R. Bedside Obstetrics and Gynecology 1st Edition. 2010.
2. Report on the Confidential Enquiries into Maternal Deaths in Malaysia. 2006-2008.
3. World Health Organization, Maternal and Perinatal Death Reviews in UK, Retrieved January 2, 2018.
4. World Health Organization, Malaysia’s Experience with Maternal Deaths. Retrieved January 24, 2018.
5. Hashim N, Naqvi S, Khanam M, Jafry HF. Primiparity as an intrapartum obstetric risk factor. J Pak Med Association. 62: 2012.
6. Chandrika S. A study of prevalence, causes, risk factors and outcome of severe obstetrics haemorrhage. BioMedical Journal. 2008.
7. Tan AC, Leong EW, Chua AC, & Moy FM. Racial variations in booking haemoglobin of primigravidae in Malaysia: A prospective study. BMC Research Notes. 2013.
8. Tsu VD. Postpartum haemorrhage in Zimbabwe: A risk factor analysis. Obstet Gynaecol Journal. 1993.
9. Carlos Montufar Rueda, Laritza Rodriguez, Jose Douglas Jarquin, Alejandra Barboza Flor Marin. Severe Postpartum Hemorrhage from Uterine Atony: A Multicentric Study. Journal of Pregnancy. 2013.
10. Koblinsky M, Campbell O, Harlow S. The Health of Women: A Global Perspective. Journal of Public Health Policy. 1995.
11. Third- or fourth-degree tear during childbirth RCOG guideline.
12. Halle-Ekane G, Emade F, Bechem N, Palle J, Fongaing D, Essome H et.al. Prevalence and Risk Factors of Primary Postpartum Hemorrhage after Vaginal Deliveries in the Bonassama District Hospital, Cameroon. International Journal of Tropical Disease& Health. 2015; 13: 1-12.
13. Smith LA, Price N, Simonite V, Burns EE. Incidence of and risk factors for perineal trauma: A prospective observational study. BMC Pregnancy and Childbirth. 2013; 13.
14. Djokovic D, Costa C, Martins A, Abushad S. Spontaneous delivery through a cervical tear without cervical so dilatation. Clinical Case Reports. 2014; 3: 3-6.
15. Sapkal R. Chapter-03 Internal Iliac Artery: A Study on Cadaver. Surgical Skills on Internal Iliac Artery Ligation for Controlling Postpartum & Pelvic Hemorrhage. 2015; 19-38.
16. Nyflot LT, Stray-Pedersen B, Forsén L, & Vangen S. Duration of labor and the risk of severe postpartum hemorrhage: A case-control study. Plos One. 2017; 12.
17. Joong LH, Norwitz ER, & Shaw J. Contemporary Management of Fibroids in Pregnancy. Rev Obstet Gynecol. 2010; 3: 20-27.
18. Waheed G, Toheed R, Mansha M. Comparison of Causes of Postpartum Haemorrhage Following Vaginal Deliveries and Caesarean Sections in a Tertiary Care Hospital of Pakistan. Pakistan Journal of Medical and Health. 2013.
19. Weeks A. The prevention and treatment of postpartum haemorrhage: What do we know, and where do we go to next? BJOG: An International Journal of Obstetrics & Gynecology. 2014; 122: 2014.
20. Pavord S, Maybury H. How I treat postpartum hemorrhage? American Society of Hematology. 2015.