Cognitive Impairment in Patients with Type 2 Diabetes Mellitus in a Primary Care Setting of a Tertiary Hospital in North Central Nigeria.
Odeigah LO1*, Rotifa SU2, Oligbu P3 and Okeke K4
1. Department of Family Medicine, Faculty of Clinical Sciences, University of Ilorin, Kwara-State, Nigeria
2. Department of Epidemiology and Community Health, Federal Medical Center, Yenagoa, Bayelsa-State, Nigeria
3. Department of Family Medicine, University of Benin Teaching Hospital, Benin-City, Edo-State, Nigeria
4. Federal Polytechnic Medical Center, Bida, Niger State, Nigeria
Corresponding author:
Odeigah LO, Department of Family Medicine, Faculty of Clinical Sciences, University of Ilorin, Kwara-State, Nigeria
Received: October 1, 2021
Accepted: October 10, 2021
Published: October 11, 2021
1. Abstract
1.1.Background: Cognitive impairment is increasing worldwide with its burden affecting a wide range of adults. It is a less addressed and underdiagnosed complication of Diabetes Mellitus. This study aimed to determine the prevalence and pattern of cognitive impairment among type 2 diabetic patients in the primary care setting of a tertiary hospital. It also determined the relationship between cognitive impairment and socio-demographic factors among participants. Materials and Method: It was a descriptive hospital-based cross-sectional study. Data was collected from 274 adult type 2 diabetic patients attending the Family Medicine clinics of the University of Ilorin Teaching Hospital, Ilorin in North Central Nigeria from March through May 2017. Interviewer-administered structured and semi-structured questionnaires were used to obtain information from the respondents. The Mini-Mental State Examination (MMSE) was used to assess the prevalence and pattern of cognitive impairment among the respondents. Data was collated and analyzed using the Statistical Package for Social Sciences version 21 (SPSS-21). Results: The prevalence of cognitive impairment in this study was 27%. Mild cognitive impairment was commoner than severe cognitive impairment. Cognitive impairment had a statistically significant relationship with the age, level of education and employment status of the respondents (p-values of 0.001, 0.026 and 0.014 respectively). Conclusion: Cognitive Impairment is common among type 2 diabetic patients in primary care. Primary Care Physicians should routinely screen type 2 diabetic patients for cognitive impairment as well as assess its pattern and risk factors. This would allow for the implementation of appropriate care to prevent cognitive impairment or its worsening among type 2 diabetic patients.
1.2.Keywords: Cognitive impairment; Type 2 Diabetes Mellitus; Mini-Mental State Examination; Primary Care.
Introduction
Cognition is a combination of mental processes that includes the ability to learn new things, intuition, judgment, language, and remembering [1]. Cognitive impairment (CI) is when a person has difficulty remembering, learning new things, concentrating, or making decisions that affect everyday life [2]. It is a major health problem, worldwide, and every 7 seconds, a new case of dementia, a severe form of cognitive impairment, is diagnosed [3]. About 50 million people have dementia worldwide, with nearly 60% of them living in low and middle-income countries [4]. Cognition assessment has not been given much priority as between 40% and 80% of cases of dementia are undiagnosed in the primary care setting, and consequently do not get well managed [5].
Cognitive impairment ranges from the mild to severe the form [2]. With mild impairment, people may begin to notice changes in cognitive function but are still able to do their everyday activities [2]. Severe cognitive impairment, as seen in dementia, can lead to losing the ability to understand the meaning or importance of something and the ability to talk or write, resulting in inability to live independently [2]. It can affect memory, thinking, orientation, comprehension, calculation, learning capacity, language, and judgement [4]. Cognitive impairment has caused an increase in morbidity in type 2 diabetic patients with varying pattern of impairment, as found in various studies [6-8]. Mild cognitive impairment has been reported to be commoner than the severe form in Nigeria [6-7].
Diabetes mellitus is a complex metabolic disease that can have devastating effects on multiple organs in the body [9]. Type 2 diabetes occurs in about 90% of people with diabetes around the world [10]. Diabetes is a common cause of nephropathy, visual loss, neuropathy, and cardiovascular disease [9]. A less addressed and not as well recognized complication of diabetes is cognitive impairment. It is more prevalent and more severe in patients with diabetes than in non-diabetic patients, with the estimated risk being 20% to 70% higher in the presence of diabetes [3]. Cognitive impairment may interfere with diabetes self-management and poor diabetes control may contribute to cognitive decline [8].
In the primary care setting, there is a need to increase training in the clinical assessment of patients so that clinicians are more aware of cognitive impairment and can deliver a timely diagnosis [8]. Severe forms of cognitive impairment are an important source of family burden. Thus, there is an obvious need to promote help-seeking among patients and to improve the awareness of clinicians so that they detect more cases. Also, the early identification of clinically relevant cognitive impairment in diabetic patients is essential because of available symptomatic treatment, the need to educate patients and caregivers to institute required supportive measures [13-14].
Materials and Method
This descriptive cross-sectional study was conducted at the Family Medicine department of the University of Ilorin Teaching Hospital (UITH), Ilorin in Kwara State, Nigeria.
The study population consisted of 274 consenting adult patients aged at least 18 years with type 2 Diabetes Mellitus attending the General Outpatient Clinics of the department. In order to determine this minimum sample size the accuracy, confidence level and prevalence rates were considered. A prevalence of 21.7% in a study by Ugoya et al in Jos Nigeria was used for the sample size calculation. Systematic random sampling technique was used to recruit eligible participants. Excluded from the study were patients with type 1 diabetes and gestational diabetes; acutely ill patients who were too ill to participate in the study; and patients with other psychiatric disorders as this may affect the assessment of cognitive function. The financial burden involved in the execution of this research was borne by the researcher. In accordance with the Helsinki Declaration, the study was approved by the Ethical Review Committee of the University of Ilorin Teaching Hospital, Ilorin while each participant voluntarily gave informed consent.
Data collection
Data was collected using structured and semi-structured interviewer-administered questionnaires.
Cognitive assessment was done with the Mini-Mental State Examination (MMSE).
The MMSE was developed by Folstein et al in 1975 to assess mental status. It is an 11-question measure that tests five areas of cognitive function: orientation, registration, attention, recall, and language [15]. The maximum score is 30. A score of 24 -30 is normal, 18-23 is indicative of mild cognitive impairment and less than 18 is indicative of severe cognitive impairment [15]. All domains of the MMSE were assessed in this study.
Data analysis
The collected data was sorted, coded and entered into the computer for analysis using the Version 21 software packages of the Statistical Package for the Social Sciences (SPSS® v21). Results were presented using frequency tables and charts. Chi-square was used to assess the associations between socio- demographic variables and cognitive impairment. The level of significance of this study was set at less than 5% (p <0.05).
Results
Socio-demographic Characteristics of the Participants
A total of 274 type 2 diabetic patients attending the Family Medicine Department of UITH Ilorin participated in the study. Table 1 shows the socio-demographic characteristics of the respondents. The mean age of participants was 60 ± 9.8. A greater percentage of the respondents 94 (34.3%) were between 50-59 years of age. The gender distribution revealed a preponderance of female respondents of 196 (71.5%), while the male respondents numbered 78 (28.5%) with a female to male ratio of 2.5:1.
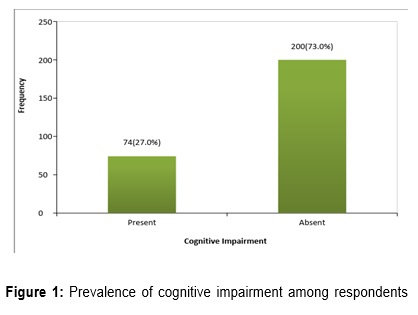
Prevalence Of Cognitive Impairment Among Respondents
As shown in Figure 1, the prevalence of Cognitive Impairment among the participants was 27%.
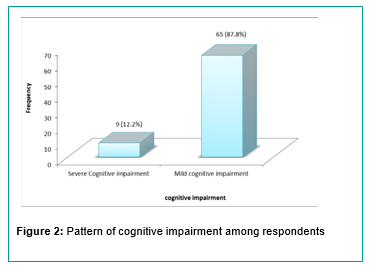
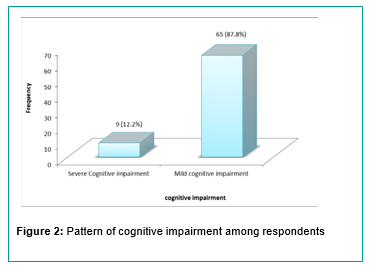
Pattern Of Cognitive Impairment Among Respondents
Association Between Cognitive Impairment And Socio-Demographic Variables Table 2 below shows the association between socio- demographic variables and cognitive impairment. Cognitive imp
Association Between Cognitive Impairment And Socio-Demographic Variables
Table 2 below shows the association between socio- demographic variables and cognitive impairment. Cognitive impairment was highest in the age group greater than 70 years (45.9%) and was absent in the age group less than 39 years (0.0%). Similarly, cognitive impairment was commonest among participants with no formal education (39.7%) and least among participants with tertiary education (16.5%). Cognitive impairment was also highest among self-employed participants (33.3%) compared to: civil servants (10.4%); the unemployed (30.4%); and others (20.5%). These associations were statistically significant with p-values of 0.001, 0.026 and 0.014 respectively
Discussion
In this study, the prevalence of cognitive impairment was found to be 27%. This means that approximately, one out of every four type 2 diabetic patients have cognitive impairment. This is comparable to the findings by Ugoya et al in Jos which is also in the North-Central region of Nigeria where the prevalence of cognitive impairment among diabetic patients was reported as 21.7% [7].
The prevalence of cognitive impairment in this study was however lower than the findings by Eze et al in Abakaliki, Eastern Nigeria, in their study among 450 type 2 diabetic patients and that of Mukheerji et al in a hospital-based cross- sectional study among 50 diabetic patients in West Bengal, India with prevalence rates of 40% and 42% respectively [6- 16]. It is also different from the findings by Kataria et al in a hospital-based study among 102 type 2 diabetic patients in Gujarat, India where a prevalence of 35% was found [17]. Also, the prevalence of cognitive impairment found in this study was higher than that found by Gao et al in a community-based study among 8,213 participants in Tianjin, China, where a prevalence of 15.85% was found [18]. A possible reason for the differences in the findings of the above studies from this study could be the methodology involved in the studies.
The finding of this study showed that cognitive impairment is common among type 2 diabetics in the Family Medicine clinics of the University of Ilorin Teaching Hospital. This is not surprising as Diabetes Mellitus has been shown to have both degenerative and vascular effects on the brain, causing a reduction in cognition [9-19]. Also the added effects of co- morbidities that occur with diabetes could increase impaired cognition [6-20].
The majority of the participants with cognitive impairment had the mild form. This is comparable to the findings by Ugoya et al in Jos, Nigeria where the majority of the participants with cognitive impairment had the mild form [7]. The findings in this study are also comparable with the findings by Kataria et al in Gujarat, India and Gao et al in China where a majority of those with cognitive impairment had the mild form [17-18].
This trend shows the need for proper evaluation and adequate management of patients with risk factors for cognitive impairment. This will prevent progression to the severe form of cognitive impairment, and bring about improvement in the quality of life of the patients.
The prevalence of cognitive impairment increased as age increased in this study with the highest proportion found among the age group greater than 70 years. The finding of an increasing prevalence of cognitive impairment with age in this study is similar to the findings by Eze et al in Abakaliki Nigeria [6]. It is also comparable to the findings by Gao et al in China and Umegaki et al in Japan, who also found an increase in cognitive impairment with age among diabetics [18-21]. Gureje et al in a community-based cohort study among 2,149 participants with age above 65 years in Ibadan, Nigeria and Harada et al in Birmingham, also reported a similar pattern among the general population [22-23].
The finding in this study could be because increasing age has been reported as a risk factor for increasing neurodegenerative changes in the brain causing cognitive impairment [23]. Also, the occurrence of causal factors for vascular diseases, such as diabetes, has been reported to increase with age. Such vascular conditions could lead to both large and small vessel diseases leading to possible brain lesions such as infarcts and consequent cognitive impairment [25].
The level of education was found to have a statistically significant relationship with cognitive impairment. This is similar to the findings by Eze et al in Abakaliki, eastern Nigeria where low educational attainment was associated with a higher prevalence of cognitive impairment [6]. The findings in this study are however different from those by Wilson et al in a longitudinal study among 6,000 elderly people of a community in the south of Chicago, where the educational level was not associated with cognitive decline [26]. The findings in this study may imply that a low level of education is a risk factor for cognitive impairment as seen in a study by Sharp et al [27].
Employment status was found to have a statistically significant relationship with cognitive impairment as cognitive impairment was commoner among the self-employed and least among the civil servants. This is comparable to the findings by Eze et al in Abakaliki where cognitive impairment was more common among traders, farmers, and artisans and least prevalent among the civil servants [6]. The findings in this study and that of the study in Abakaliki could be because among the self-employed were petty traders and artisans who were mainly individuals with primary or no formal education which is a risk factor for cognitive impairment [6-27].
This study had some limitations. It was a descriptive cross-sectional study and therefore the outcome may not necessarily carry a causal relationship with the tested variables. A longitudinal study design would be required to establish causal relationships. It is however intended to add to the body of knowledge that will form a template for future studies. Also, the hospital-based nature of the study could have exaggerated the true burden of cognitive dysfunction in patients with type 2 diabetes mellitus, hence the findings are not generalizable. There is a need for a community-based study with a larger sample size to determine the effect of type 2 Diabetes Mellitus on cognitive function
Conclusion
The prevalence of cognitive impairment was 27% in this study, with about one in every four participants having cognitive impairment. Mild cognitive impairment was the most common pattern seen in the study. Cognitive impairment was found to have a statistically significant association with age, level of education and employment status. Physicians in primary care should ensure screening of patients with diabetes mellitus for cognitive impairment to detect early cases, manage appropriately and avoid where possible the progression of the disease. Physicians should also ensure adequate patient counselling on proper ways to ensure the care of the aging population as the prevalence of cognitive impairment was shown to increase with age in this study. The level of education and employment status should also be assessed and patients evaluated appropriately and managed for cognitive impairment if present. This is important in primary care, as Family Medicine offers first contact care and provides comprehensive and lifelong care to the patient irrespective of age, sex or disease condition.
References
1. Center for disease control and prevention. Healthy aging. 2017. https://www.cdc.gov/aging/healthybrain/index. htm. Accessed: 10, January 2018.
2. Center for disease control and prevention. Cognitive impairment: A Call for action now. 2011. http://www.cdc.gov/ aging/healthybrain/index.htm. Accessed: 15, August 2017.
3. Koekkoek PS, Kappelle LJ, van den Berg E, Rutten GE, Biessels GJ. Cognitive function in patients with diabetes mellitus: guidance for daily care. Lancet Neurol. 2015;14:329– 40. doi: 10.1016/S1474-4422(14)70249-2.
4. World Health Organization. Dementia. 2017. http:// www.who.int/mediacentre/factsheets/fs362/en/. Accessed: 14, November 2017.
5. Connolly A, Gachi E, Martin H, Morris J, Purandare N. Underdiagnosis of dementia in primary care: variations in the observed prevalence and comparisons to the expected prevalence. Aging Ment Heal. 2011;15(8):978–84. doi: 10.1080/13607863.2011.596805.
6. Eze OC, Basil CE, Uma AK,Onwuekwe OI. The Prevalence of Cognitive Impairment Amongst Type 2 Diabetes Mellitus Patients at Abakaliki, South East Nigeria. J Diabetes Metab Syndr Disord. 2015;1(1):1–3. doi: 10.4172/2167- 0943.1000171.
7. Ugoya SO, Agaba EI, Ladep NG, Puepet FH, Ogunniyi A. Cognitive Dysfunction in Diabetes Mellitus in Jos, North- Central Nigeria. Hungarian Med J. 2008;2(2):215–9. doi: 10.1556/HMJ.2.2008.2.4.
8. Ohara T, Doi Y, Ninomiya T, Hirakawa Y, Hata J, Iwaki T et al. Glucose tolerance status and risk of dementia in the community. Neurology. 2011;77(12):1126–34. doi: 10.1212/WNL.0b013e31822f0435.
9. Kodl CT, Seaquist ER. Cognitive dysfunction and diabetes mellitus. Endocr Rev. 2008;29(4):494–511. doi: 10.1210/er.2007-0034.
10. World Health Organization. Diabetes. 2018; http:// www.who.int/mediacentre/factsheets/fs138/en/. Accessed: 02, February 2018.
11. Hopkins R, Shaver K, Weinstock RS. Management of adults with diabetes and cognitive problems. Diabetes Spectr. 2016;29(4):224–37. Diabetes Spectrum 2016 Nov; 29(4): 224- 237. https://doi.org/10.2337/ds16-0035.
12. Edwards R, Voss S, Iliffe S. Education about dementia in primary care: is person-centredness the key? Dementia. 2014;13(1):111–9. doi: 10.1177/1471301212451381.
13. Alzheimers Association. What is dementia? 2016; http:// www.alz.org/what-is-dementia.asp. Accessed: 14, January 2017.
14. Bradford A, Kunik ME, Schulz P, Williams SP, Singh H. Missed and delayed diagnosis of dementia in primary care: prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009;23(4):306–13. doi: 10.1097/ WAD.0b013e3181a6bebc.
15. Folstein MF, Folstein SE, McHugh PR. Mini-Mental State” a Practical Method for Grading the Cognitive State of Patients for the Clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6
16. Mukherjee P, Mazumdar S, Goswami S, Bhowmik J, Mukhopadhyay S, Jana S, et al. Cognitive Dysfunction in Diabetic Patients With Special Reference to age of onset. Act Nerv Super (Praha). 2012;54(1):67–75. https://doi. org/10.1007/BF03379585.
17. Kataria L, Pandya H, Shah S, Shah H, Gerg R. Prevalence and Pattern of Cognitive Dysfunction in Type 2 Diabetes Mellitus. Int J Med Appl Sci. 2013;2(4):245–52.
18. Gao Y, Xiao Y, Miao R, Zhao J, Cui M, Huang G, et al. The prevalence of mild cognitive impairment with type 2 diabetes mellitus among elderly people in China: A cross- sectional study. Arch Gerontol Geriatr. 2016;62:138–42. doi: 10.1016/j.archger.2015.09.003.
19. Hiroyuki U. Pathophysiology of cognitive dysfunction in older people with type 2 diabetes : vascular changes or neurodegeneration ? Age Aging. 2010;39:8–10. doi: 10.1093/ ageing/afp211.
20. Sabia S, Kivimaki M, Shipley MJ, Marmot MG, Singh- Manoux A. Body mass index over the adult life course and cognition in late midlife: The Whitehall II Cohort Study. Am J Clin Nutr. 2009;89(2):601–7. doi: 10.3945/ajcn.2008.26482.
21. Umegaki H, Kawamura T, Kawano N, Umemura T, Kanai A, Sano T. Factors Associated with Cognitive Decline in Elderly Diabetics. Dement Geriatr Cogn Disord Extra. 2011;1:1–9. doi: 10.1159/000323188
22. Gureje O, Ogunniyi A, Kola L, Abiona T. Incidence of and risk factors for dementia in the Ibadan study of aging. J Am Geriatr Soc. 2011;59(5):869–74. doi: 10.1111/j.1532- 5415.2011.03374.x.
23. Harada CN, Love MCN, Triebel K. Normal Cognitive Aging. Clin Geriatr Med. 2013;29(4):737–52. doi: 10.1016/j. cger.2013.07.002.
24. Egbi OG, Ogunrin O, Oviasu E. Prevalence and determinants of cognitive impairment in patients with chronic kidney disease: A cross-sectional study in Benin City, Nigeria. Ann Afr Med. 2015;14(2):75–81. doi: 10.4103/1596- 3519.149877
25. Iemolo F, Duro G, Rizzo C, Castiglia L, Hachinski V, Caruso C. Pathophysiology of vascular dementia. Immun Ageing. 2009;6(13):1–9. doi:10.1186/1742-4933-6-13.
26. Wilson RS, Hebert LE, Scherr PA, Barnes LL, De Leon CFM, Evans DA. Educational attainment and cognitive decline in old age. Neurology. 2009;72(5):460–5. doi: 10.1212/01. wnl.0000341782.71418.6c
27. Sharp ES, Gatz M.Relationship between education and dementia: an updated systematic review. Alzheimer Dis Assoc Disord. 2011;25(4):289–304. doi: 10.1097/ WAD.0b013e318211c83c.