Evaluation of Systolic Function of the Right Ventricle in Patients with Chronic Obstructive Pulmonary Disease: A Cross Sectional Study about 30 Cases.
Alassane NA1*, Diaba GN2, Antoine SS3, Fatou AW3, Momar D4, Maimouna SOW3, Malick B3, Bamba NM3, Alassane M1, Abdoul K2
1. Cardiology Department of Grand Yoff General Hospital, Dakar, Senegal
2Cardiology Department of Dalal Djam Hospital, Dakar Senegal
3Cardiology Department of Aristide Le Dantec Teaching Hospital, Dakar, Senegal
4Cardiology Department of Fann Hospital, Dakar, Senegal
Corresponding author:
NGAIDE Aliou Alassane, Cardiology Department of Grand Yoff General Hospital, Dakar, Senegal
Received: September 07, 2021
Accepted: September 14, 2021
Published: September 20, 2021
1. Abstract
1.1. Introduction: Chronic pulmonary heart is the main cardiovascular complication of chronic obstructive pulmonary disease. The aims of our study were to evaluate the right ventricular systolic function in patients with chronic obstructive pulmonary disease and to investigate the relationship between parameters of right ventricular function and pulmonary function testing data. Methodology: A multicenter cross-sectional study was conducted between January 2013 and July 2013 in cardiology and pulmonology department in Dakar. Was included all in or outpatient diagnosed for chronic obstructive pulmonary disease. Results: 30 patients were evaluated in this cohort. The mean age was 62.4 years. Male predominance was noted (sex ratio of 9). Right heart failure was found in 7 patients (23.3%). Right ventricule enlargement was noted in 12 patients (40%). Mean sPAP was 58.58 ± 23.59 mmHg. Pulmonary arterial hypertension was found in 16 (53.3%) patients. TAPSE was i the systolic pulmonary arterial pressure (sPAP) value greater than 60 mm Hg, as you choose as a cut-off for pulmonary hypertension mpaired in 7 patients (23.3%). Reduction of right ventricule fractional area change was present in 14 (46.6%) patients. S’ of the tricuspid annulus velocity was reduced in 11 (33%) patients. Parameters correlated with the severity of chronic obstructive pulmonary disease were: TAPSE (p= 0.0099), right ventricule fractional area change (p = 0.0095), S’ of the annular tricuspid (p= 0.0173) TEI index (p= 0.038) and Pulmonary arterial hypertension (p= 0,023). Conclusion: Evaluation of right ventricular systolic function in chronic obstructive pulmonary disease is fundamental and must use multiple parameters.
1.2. Keywords: COPD; Systolic Function of the Right Ventricle; Senegal.
Introduction
The study of the right ventricle has seen a renewed interest in recent years in many pathologies. Unfortunately, even if its prognostic importance is no longer to be proven, the evaluation of the systolic function of the right ventricle is still not systematic. The chronic pulmonary heart (CPC) and right ventricular dysfunction are considered to be the main cardiovascular complications during chronic obstructive pulmonary disease (COPD) [1,2]. They mark a turning point in the evolution of respiratory disease and conditions the establishment of specific therapies. It is therefore essential to look for a cardiac impact by clinical examination and cardiac Doppler ultrasound [2].
In Senegal, few studies have been devoted to the cardiovascular manifestations of COPD. The objectives of our study were:
- to assess the systolic function of the right ventricle in patients with chronic obstructive pulmonary disease, at different stages of disease severity;
- to analyze the relationship between the different echocardiographic parameters of right ventricular systolic function and the degree of severity of COPD.
Methodology
IThis is a cross-sectional, descriptive, multicenter study, conducted from January 2013 to July 2013 carried out in the pulmonology departments of the FANN University Hospital Center and the cardiology departments of the Aristide Le Dantec CHU.
Included was any hospitalized or outpatient patient for COPD with or without evidence of heart dysfunction or exacerbation of COPD. The patients benefited from a complete clinical examination as well as a paraclinical assessment (biological parameters, electrocardiogram, chest chest X-ray, EFR, echocardiography).
Doppler echocardiography made it possible to measure the cavity dimensions, the systolic function of the Left Ventricle (LV) but especially of the Right Ventricle (RV). Several parameters of the systolic function of the RV were used: the Tricuspid Annular Plane Excursion (TAPSE), the Fraction of Shortening of the LV (FSLV), the longitudinal speed or peak of the Sa tricuspid wave, the isovolumic acceleration, the TEI index and max dP/dt index. The LV eccentricity index corresponding to the ratio of the anteroposterior and septo-lateral diameter of the left ventricle was measured on a mid-ventricular minor axis section, in telesystole and telediastole.
The diastolic function of the RV was also appreciated. The pulmonary arterial pressure was evaluated by Doppler by the flows of tricuspid insufficiency and/or pulmonary insufficiency. A value below 35 mm Hg was considered normal, however age is taken into account [3]. Pulmonary Arterial Hypertension (PAH) was severe for a systolic pulmonary arterial pressure (sPAP) value greater than 60mm Hg. The standards for the various echocardiographic parameters studied were those recommended by the American Society of Echocardiography (ASE) as shown in Table 1 [3]. A systematic Respiratory Functional Exploration (RFE) made it possible to explore the pulmonary ventilatory function in search of an obstructive, restrictive or mixed syndrome and to assess its severity using the GOLD classification [4].
Rvd: Right Ventricle Diastolic Diameter; Lv: Left Ventricle; Tdd: Telediastolic Diameter; Sf: Shortening Fraction; Ef: Ejection Fraction; Ivc: Inferior Vena Cava; Ra: Right Atrium; Itvt: Integral Tricuspid Velocity Time; Itvp: Intégral Pulmonary Velocity Time.
All of the data collected was entered by the Epi data software and analyzed with SPSS 16.0 and Excel software. The description of the qualitative variables was done using percentages and that of the quantitative variables using means and standard deviations. Chi2 and Fisher tests allowed the comparison of proportions. A value of p <0.05 was considered as a threshold of statistical significance.
Results
A total of 30 patients were included over a period of 6 months 15 days. The average age of the patients was 62.4 years [40-83 years]. The age group included [50-64 years] represented 53.3%. The male gender was predominant and represented 90% of the population. The sex ratio (male/female) was 9. A history of pulmonary tuberculosis was found in 5 cases and that of pulmonary embolism in one patient. The average duration of evolution of COPD was 5.08 years.
Signs of right heart failure were found in 23.3% of cases. The average hemoglobin level was 17g/dl. On the electrocardiographic level, a sinus rhythm was found in 27 patients (90%). The electrocardiogram (ECG) was normal in 6 patients (20%). The anomalies were dominated by the right atrial hypertrophy found in 43.3% of the cases (Table 2,3).
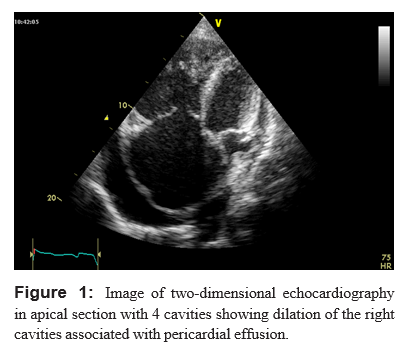
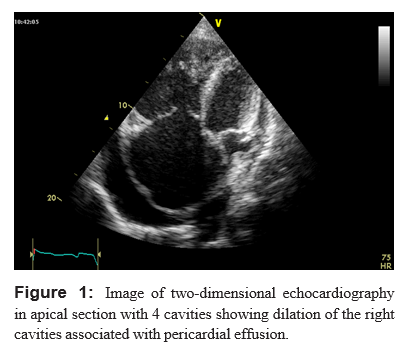
Echocardiographically, the right ventricle was dilated in 12 patients, ie 40% of the cases (Table 4); the same was true for the right atrium (Figure 1). Nine patients presented with echocardiographic signs of chronic pulmonary heart. There was left atrial and ventricular dilation in 7 cases (23.33%) and 3 cases (10%), respectively. Left ventricular systolic function was impaired in 4 (13.3%) patients. sPAP was measured in 27 patients. Its average was 58.58 mmHg. PAH was noted in 20 patients (74%). It was severe in 13 patients, moderate and mild in 5 and 2 patients, respectively. There was a significant correlation between the presence of PAH and the stage of severity of COPD (p = 0.023).
The average index of eccentricity in telesystole was 1.255; that in telediastole of 1.33. An increase in both indices, witnessing a barometric overload, was noted in 12 (40%) of our patients. Diastolic DV function was abnormal in 12 cases (40%). No cases of relaxation disorder were found. We had 9 cases of pseudo-normal aspect and 3 cases of restrictive disorders. The results of the evaluation of the systolic function parameters were a function of the sPAP and of the existence or not of an exacerbation (Table 5).
The TAPSE was altered in 7 patients and the mean found was 18.20mm. Its alteration was significantly correlated with the stage of COPD (p = 0.0099). The RV shortening fraction was impaired in 14 patients (46.6%), with an average of 34.95% ± 10.12. The alteration was significantly correlated with the stage of COPD (p-0.0095). The Sa tricuspid index was altered in 11 patients (33%) and was significantly correlated with the stage of COPD (p = 0.0173).
The isovolumic acceleration was abnormal in 6 (20%) of our patients, and not correlated at the stage of COPD (p = 0.09). The TEI index could be calculated in 23 patients and was abnormal in 17 (73.9%) patients. Its mean value was 0.60 and it was significantly correlated with the severity of COPD (p = 0.038). The dP/dt index could be assessed in 16 patients. It was less than 400mmHg/s in 5 of them (26%) and not correlated at the stage of COPD (p = 0.3296), with an average of 539.5mmHg/s. Thirteen patients, or 43% of the study population, had an impairment of at least three of the systolic function indices.
The data collected from the RFE made it possible to classify the patients according to the progressive stage of COPD (Table 6).
Two patients had an improvement in their sub-bronchodilator numbers, no total reversibility was noted
Discussion
The prevalence of right heart failure in our study was 23.3%. Gūder G [5] found a prevalence of 17%. Right atrial hypertrophy and RV hypertrophy were present in 43.3 and 36.6% of the cases, respectively. These two electrocardiographic signs were mainly found when the stage of COPD was advanced; a finding found in the study of Sharma et al [6] and in that of Warnier et al [6,7], more, Holtzman et al [8] demonstrated that the sensitivity, specificity, positive and negative predictive value of the ECG relating to RVH in COPD were 50%, 100%, 100%, and 75%, respectively. The chest chest X-ray showed cardiomegaly and signs of PAH in 40% and 20% of the cases, respectively. Himelman et al [9] found cardiomegaly and signs of PAH in 18% and 21% of their patients, respectively. Gupta S et al [10] found 20% cardiomegaly and 36.6% signs of PAH. We found left ventricular dysfunction in Simpson biplane in 4 (13.3%) patients and longitudinal systolic dysfunction in 5 patients (16.6%). The mean EFLV value for the Simpson biplane was 63%; and the results obtained in other studies seem, on the whole, similar to those described in the literature [11-13].
Left ventricular dysfunction during COPD is due to many factors, such as hypoxemia and acidosis, involvement of the coronary arteries, or ventricular interdependence. In addition, some studies claim that if LV systolic dysfunction is possible during COPD without PAH, it worsens with the value of PAPS [10,14]. Nine patients (30%) had echocardiographic signs of chronic pulmonary heart. Gupta [10] and Maula [15] found 17.5% and 32.7% respectively during their studies. The alteration of the diastolic function of the RV, found in 40% of the cases, would be related to the hypertrophy/dilation of the latter. The study by Tei et al [16] effectively shows that PAH leads to an impairment of the systolic and diastolic function of RV; this was confirmed by Vizza et al [17] who highlighted the diastolic dysfunction of RV during COPD. We found PAH in 72.7% of cases as well as a positive correlation between the stage of COPD and PAH. Gupta [10] and Maula [15] found 42.5% and 65.4% respectively of patients who had PAH, and also found a significant correlation between the stage of COPD and the severity of PAH. This correlation can be explained by that which exists between variations in PaO2 and pulmonary arterial pressure [18]. There is a monumental worsening of PAH during episodes of exacerbation of COPD which is explained by the worsening of hypoxemia and hypercapnia [2,19]. The right ventricular function ultrasound assessment is complex due to the anatomy and position of the LV, thus requiring the combination of several parameters.
During our study, we were able to highlight a relation between the deterioration of the indices of systolic function of the RV and the stage of the COPD and the presence or not of signs of clinical exacerbation on the one hand, and the presence and the severity of PAH on the other hand. In fact, if we compare a group of patients with mild to moderate COPD to that of severe to very severe COPD, the impairment of SFRV is significantly more marked in the moderate to severe COPD group (p = 0.0095). This correlation is significant for TAPSE (p = 0.0099), Sa tricuspid (p = 0.0173) and the Tei index (p = 0.038), but not significant for isovolumic acceleration (p = 0.09). Concerning the Tei index, if its alteration seems more marked in patients with PAH (0.71 + 0.42), it seems less sensitive to the presence or not of an exacerbation, with an average of 0, respectively. 61 ± 0.40 and 0.59 ± 0.37.
Botelho [19] as well as Ozben [20] also found, by comparing the results before and after the treatment of the COPD exacerbation, a relatively stable Tei index, but there was a significant difference notably for the isovolumic acceleration [20] (p = 0.013). The alteration of at least 3 indices of the systolic function of RV in the same subject was present in 62.5% of patients with severe or very severe COPD against 21.4% of cases of mild to moderate COPD (p = 0.0235 ).
Right ventricular systolic dysfunction is commonly associated with PAH. Moreover, the recommendations issued by the European Cardiology Society [21] on the diagnosis of PAH in ultrasound, confirm the need to assess the right ventricular function in PAH. Concerning the disparity of the results obtained between the indices used during our study, it would be linked to the fact that all the parameters of evaluation of the right ventricular function, starting with the EFRV which is however considered as the “gold standard”, are very sensitive to load conditions. Indeed, there is no real parameter of contractility of the RV which is independent of it, apart from perhaps the pulmonary elastance measured from the pressure/volume loops in hemodynamics [22]. In addition, if the TAPSE has already shown its interest in the evaluation of the EFRV with an excellent correlation coefficient between the TAPSE and the EFRV, it has however limits linked to the fact that the evaluation relates only to the longitudinal function of the free wall of the RV, without taking into account the contribution of the interventricular septum, the radial function, or the circumferential function, whereas these could have an important role in maintaining the right ventricular function when the contraction longitudinal decreases [23]. Finally, if the SFRV is well correlated with the EFRV evaluated by myocardial MRI and is superior to other two- dimensional evaluation methods [24], it also has the main advantage of taking into account the participation of the interventricular septum. However, the numerous RV trabeculations make it difficult to define the endocardium and are therefore a source of bias [25].
Conclusion
For the past few years, we have known the prognostic importance of RV dysfunction, especially in COPD. The estimation of the right cardiac repercussion is essential because it marks an evolutionary turning point in the evolution of respiratory disease.
References
1. WHigham MA, Dawson D, Joshi J, Nihoyannopoulos P, Morrell NW. Utility of echocardiography in assessment of pulmonary hypertension secondary to COPD. Eur Respir J. 2001; 17: 350- 355.
2. Weitzenblum E, Chaouat A, Ducoloné A. Hypertension artérielle pulmonaire et retentissement cardiaque droit des affections respiratoires chroniques. EMC - Cardiologie. 2005; 37: 1-11.
3. Rudski LG, Wyman W, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K et al. Guidelines for the Echocardiographic Assessment of the Right Heart in Adults: A Report from the American Society of Echocardiography Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23: 685-713
4. Global initiative for chronic obstructive lung disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2013.
5. Güder G, Rutten F H, Brenner S, Angermann CE, Berliner D, Ertl Get al. The Impact of Heart Failure on the Classification of COPD Severity. JCF. 2012; 18: 637-44.
6. Sharma R A, Hashim Z, Sharma E. Diagnosis of severity of COPD on the basis of electrocardiogram. Int J App Basic Med Res. 2013; 6: 527-530.
7. Warnier MJ, Rutten FH, Numans ME, Kors JA, Tan HL, de Boer A et al. Electrocardiographic Characteristics of Patients with Chronic Obstructive Pulmonary Disease. COPD. 2013; 10: 62- 71.
8. Holtzman D, Aronow W S, Mellana W M. Sensitivity, Specificity, Positive Predictive Value, and Negative Predictive Value of the 12-Lead Electrocardiogram in Predicting Right Ventricular Hypertrophy Diagnosed by a 2-Dimensional Echocardiogram in Patients with Moderate or Severe Chronic Obstructive Pulmonary Disease Followed in an Academic Outpatient Pulmonary Clinic. Open Journal of Cardiology. 2010; 1: 1-2.
9. Himelman RB, Struve SN, Brown JK, Namnum P, Schiller NB. Improved recognition of corpulmonale in patients with severe chronic obstructive pulmonary disease. Am J Med. 1988; 84: 891-898.
10. Gupta S, Khastgir T, Gupta MP, Sethi KK, Manoharan S. Clinical, hemodynamic and echocardiographic study in chronic corpulmonale. J Assoc Physicians India. 1989; 37: 373-376.
11. El Wahsha R A, Ahmedb M K, Yaseenb R I. Evaluation of left ventricular function in patients with chronic obstructive pulmonary disease with or without pulmonary hypertension. Egypt J Chest Dis Tuberc. 2013; 2:52-60.
12. Macchia A, Rodriguez Moncalvo J, Kleinert M, Comignani PD, Gimeno G, Arakaki D et al. Unrecognized ventricular dysfunction in COPD. Eur Respir J. 2012; 39: 51-58.
13. Sabit R, Boltona CE, Fraser AG, Edwards JM, Edwards PH, Ionescu AA et al. Sub-clinical left and right ventricular dysfunction in patients with COPD. Respiratory Medicine. 2010; 104: 1171-1178.
14. Funk GC, Lang I, Schenk P, Valipour A, Hartl S, Burghuber OC. Left ventricular diastolic dysfunction in patients with COPD in the presence and absence of elevated pulmonary arterial pressure. Chest. 2008; 133: 1354-1359.
15. Maula F, Nadeemkhan M, Adil M, aved Ullah, Abdul Rauf, Samiullah. Echocardiographic findings in chronic obstructive pulmonary disease (COPD) patients. Proc Am Thoracsoc. 2012; 5: 549-555.
16. Tei C, Dujardin K, Hodge D, Bailey KR, McGoon MD, Tajik AJ et al. Echocardiographic index of global right ventricular function. J Am Soc Echocardiogr. 1996; 9: 838-847.
17. Vizza CD, Lynch JP, Ochoa LL, Richardson G, Trulock EP. Right and left ventricular dysfunction in patients with severe pulmonary disease. Chest. 1998; 113: 576-583.
18. Weitzenblum E, Sautegeau A, Ehrhart M, Mammosser M, Hirth C, Roegel E. Long term course of pulmonary arterial pressure in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1984; 130: 993-998.
19. Botelho CMA, Pena JLB, Colosimo EA, Moreira MCV. Tissue Doppler imaging and myocardial deformation indices as markers of right ventricular dysfunction in chronic obstructive pulmonary disease exacerbation. Eur J Heart Fail. Supplements. 2008; 7: 82.
20. Ozben B, Eryuksel E, Tanrikulu MA, Papila N, Ozyigit T, Celikel T. Acute Exacerbation Impairs Right Ventricular Function in COPD Patients. Hellenic J Cardiol. 2015; 56: 324-331.
21. Galie N, Humbert L, Vachiery JL, Gibbs S, Lang I, Torbicki A et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). Eur Heart J. 2016; 37: 67-119.
22. Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: Anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008; 117: 1436-1448.
23. Forfia PR, Fisher M R, Mathai SC, Housten-Harris T, Hemnes AR, Borlaug BA et al. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med. 2006; 174: 1034-1041.
24. Anavekar NS, Gerson D, Skali H, Kwong RY, Yucel EK, Solomon SD. Two dimensional assessment of right ventricular function: an echocardiographic-MRI correlative study. Echocardiography. 2007; 24: 452-455
25. Lindqvist P, Calcutteea A, Henein M. Echocardiography in the assessment of right heart function. Eur J Echocardiogr. 2008; 9: 225-234.